Nearly 35% of people globally experience psychological stress, with even higher rates in the United States, where about 24% report extreme stress and 76% say stress impacts their physical health. You might think this is just the reality of modern living – tight deadlines, endless emails, financial pressures, and burnout. But here's what most people don't realize: this isn't just "being busy." When you experience constant tiredness, procrastination, burnout, and mental fog, many times it's not a lack of willpower or motivation – it's your brain's alarm system hijacking your ability to think clearly and function at your best.
So, what's causing this? It's a small, almond-shaped structure deep in your brain's limbic system called the amygdala. Understanding how it works and how to manage it could be the key to breaking free from the cycle of chronic stress.
When we think of stress, we often picture big, obvious moments. For example, losing a family member, losing a job, major life changes, or being diagnosed with a serious illness. While these are all incredibly stressful situations, chronic stress is different – it can occur in all sorts of everyday situations.
In short, chronic stress happens when your body's stress response system gets stuck in the "on" position. Instead of activating only during real emergencies, it starts firing during everyday situations like: checking emails, getting cut off in traffic, thinking about all of the action items left on your to-do list, or even just lying in bed with racing thoughts.
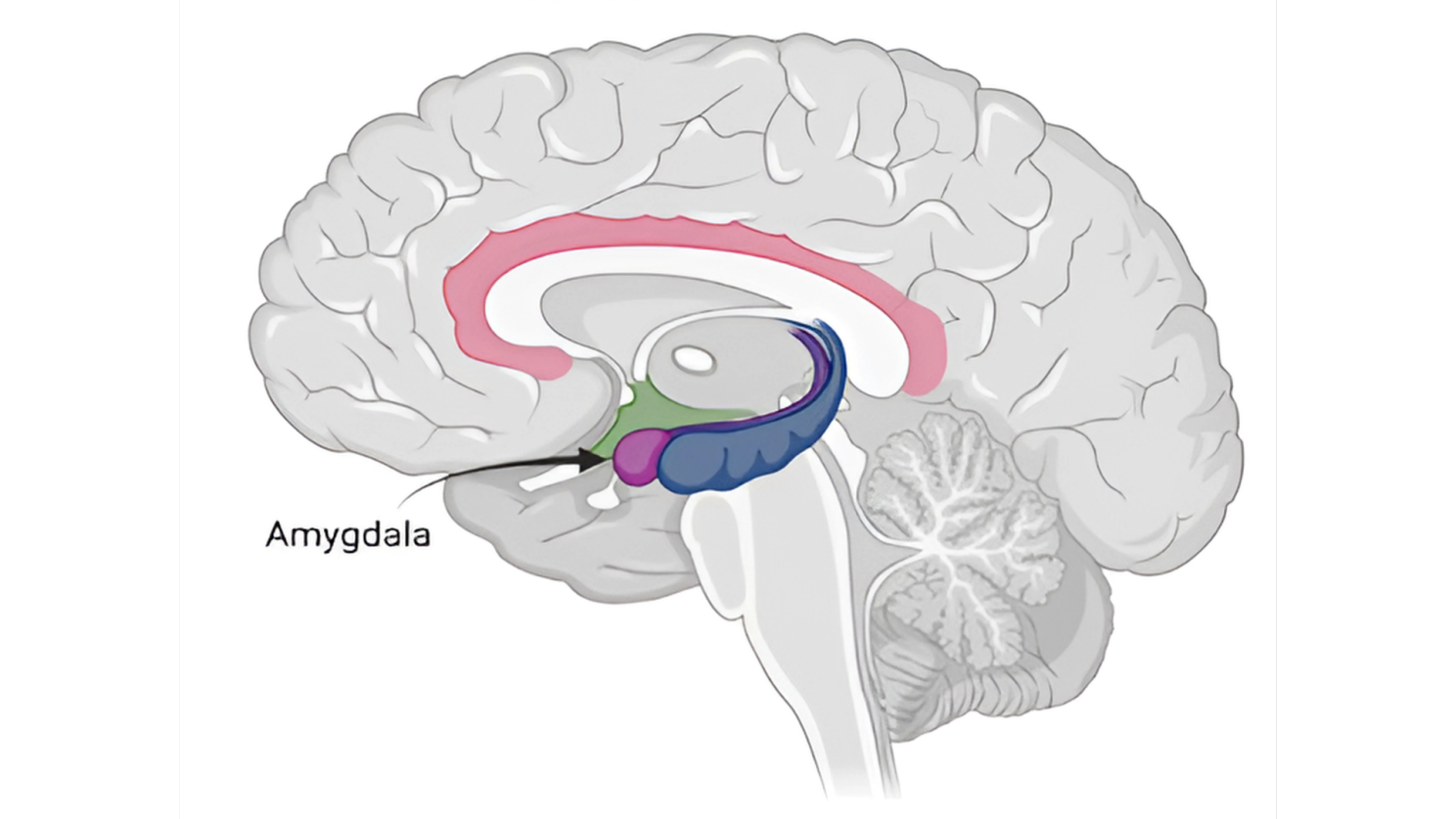
Think of your amygdala like a hypervigilant guard dog that never sleeps. This primitive part of your brain has one primary job: scan for threats and keep you alive. When it detects danger (real or perceived) it instantly triggers your fight-or-flight response. This then floods your system with stress hormones like cortisol and adrenaline.
This system worked perfectly when our ancestors faced immediate physical threats like predators. The amygdala would sound the alarm, stress hormones would be injected, and they'd either fight or run to safety. Once safe, the stress response would turn off so your body could return to equilibrium.
But here's the problem: many times your amygdala can't tell the difference between a charging bear and a passive-aggressive email. To your brain, both can trigger the same alarm system.
Today, your amygdala is constantly detecting "threats" that aren't actually life-threatening or close to being dangerous:
When your amygdala takes over, it essentially hijacks your prefrontal cortex which is the part of your brain that should be in control. This is your brain's CEO and is responsible for logical thinking and decision-making.
So when that amygdala switch is flipped on, this is why you might:

Several factors in modern life can cause your amygdala to remain in a hyperactive state:
The good news? I know it sounds like a lot of overwhelming information, but fortunately you can learn to regulate your amygdala and break the chronic stress cycle. Here are evidence-based strategies to get started:
Regular Exercise: Physical activity is one of the most effective ways to reset your amygdala and metabolize stress hormones. Exercise will help burn off cortisol and adrenaline while releasing endorphins that naturally calm your nervous system.
The 4-7-8 Breathing Technique: When you feel stress rising, breathe in for 4 seconds, hold for 7, exhale for 8. This activates your parasympathetic nervous system and signals safety to your amygdala. Practice this for just 2 minutes when you notice stress building.
Pro tip: Try humming on the exhale – this helps stimulate your vagus nerve, which has been shown to activate your parasympathetic nervous system.
The 5-4-3-2-1 Grounding Method: When overwhelmed, name 5 things you can see, 4 you can touch, 3 you can hear, 2 you can smell, and 1 you can taste. This pulls your attention away from internal threats and into the present moment.
Progressive Muscle Relaxation: Starting with your toes, deliberately tense each muscle group for 5 seconds, then release completely. Work your way up through your calves, thighs, abdomen, arms, and face. As you release each muscle group, notice the contrast between tension and relaxation. This helps discharge the physical tension that builds up when stress hormones flood your system.
Set Boundaries with Stress Triggers: Identify your specific stress triggers and create boundaries around them. This might mean checking news only once a day, turning off notifications during focused work time, setting specific hours for email, or avoiding negative news feeds first thing in the morning or right before bed.

Interestingly, there are times when you actually want your amygdala engaged. Before an athletic competition or important performance, that surge of alertness and energy can enhance your focus and reaction time. The key is learning when to turn it on intentionally and how to turn it off when you don't need it.
Managing your amygdala isn't just about feeling calmer: It's about reclaiming your cognitive abilities and living more intentionally. When your stress response is regulated:
Once these positive changes start happening, the momentum builds on itself, making it much easier to sustain these healthier patterns.
Chronic stress isn't a character flaw or a sign of weakness. At the end of the day, almost every human being will experience at least one of these stress responses in their lifetime, so don't stress about being stressed. Your amygdala is trying to protect you, but needs your help to understand what's actually threatening and what's not.
The goal isn't to eliminate stress entirely, but to help your brain distinguish between real emergencies and everyday challenges. When you can do that, you'll find that life becomes more manageable, decisions become clearer, and you can finally leverage all of your brain's capabilities!


More Info: At WellPro, we’re building an AI-native clinical platform purpose-built to scale the next era of care: personalized, preventative, and data-driven. Our thesis is simple but bold; the future of care delivery will be patient-centered, proactive, longitudinal, and closed-loop. That demands infrastructure that can ingest multi-modal health data, generate insight, drive action, and continuously optimize based on outcomes.
We believe Agentic AI is central to making this vision real. Not just chat interfaces or “co-pilots,” but deeply embedded, goal-driven AI agents that operate within the clinical system itself, helping surface insights at the point of care, automate routine tasks, and ensure closed-loop follow-through on interventions.